Abstract
Background: Foci of high grade transformation can be elusive in follicular lymphoma (FL) as current imaging modalities do not reliably discriminate low grade disease from high grade transformation. Anthracycline containing regimens such as R-CHOP are not universally employed in the treatment of FL and are often reserved for treatment of confirmed high grade transformation, in view of their well-established benefit in this situation. We initially studied the relationship between focal splenic lesions on imaging and corresponding splenic histology in a retrospective series. The association revealed by this initial study led us to hypothesise that FL patients with focal splenic lesions on imaging may benefit from anthracycline containing regimens.
Methods: All splenectomy samples between 2000 and 2016 at The Royal Marsden Hospital were identified and seventy-two patients who had pre-splenectomy imaging with CT, PET or both, and a diagnosis of B-cell lymphoma on splenic histology were included. Cases were divided into 4 groups based on pattern of splenic uptake on imaging (focal or diffuse) and splenic histology (high or low grade lymphoma).
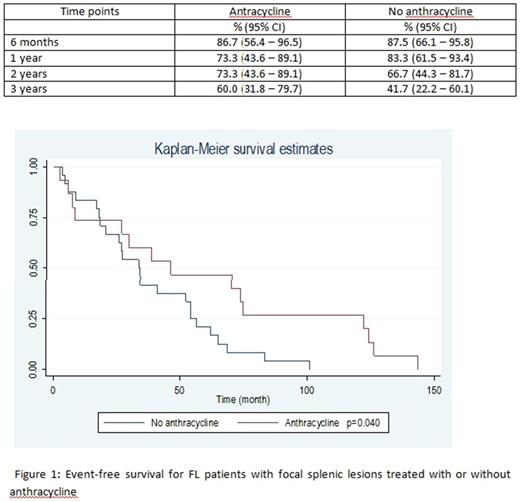
A retrospective analysis was undertaken subsequently on FL patients treated with Rituximab between January 2004 and October 2014. Over this 10 year period we identified 39 patients who were diagnosed with FL and had documented splenic lesion/s on imaging (CT and/or PET). This group was divided into those who went on to receive anthracycline based therapy and those that did not. The outcome investigated was time to event (start of another treatment and death). Kaplan Meier (KM) method was used to calculate the time to event.
Results: Of the 72 splenectomy specimens, 15 showed high grade lymphoma on histology. 14 of these cases showed focal splenic uptake by imaging. 7 of 57 low grade lymphomas showed focal splenic uptake (including hairy cell leukaemia (n = 2), FL (n = 2) and splenic marginal zone lymphomas (n = 3)). 1 of 15 high grade lymphoma showed diffuse splenic uptake and 50 of 57 low grade lymphomas showed diffuse uptake. The positive predictive value of focal splenic lesions when including raised LDH in the assessment was 77% with a negative predictive value of 98%. The sensitivity for focal lesions revealing high grade lymphoma was 93.3% with a specificity of 87.7%. The p value for the hypothesis that focal splenic lesions indicate high grade lymphomas was significant through the McNemar test at p=0.034.
Median age of the 39 patients with FL and focal splenic lesions on imaging was 69 years (range: 39 - 93). Eighteen (46%) of these patients were female. Fifteen (38%) were treated with anthracycline based treatment, the remaining 62% were not. Prior to being diagnosed with splenic lesion/s on imaging, the median number of treatments for the whole cohort was 1 (range 0 - 8). Following identification of a splenic lesion/s on imaging and subsequent treatment, the median event free survival of the overall patients was 34.2 months (95% CI: 25.6 - 54.1). In the group treated with anthracycline it was 46.0 months (95% CI: 7.3 - 74.9) versus 33.4 months (95% CI: 18.2 - 54.0) for untreated patients, with a p-value = 0.040 (Figure 1). The proportion of patients that were event free in the groups at 6 months, 1, 2 and 3 years are summarised in Table 1.
Conclusion: This study demonstrates a statistically significant relationship between focal splenic lesions on imaging and high grade lymphoma on histology with a high sensitivity and an extremely high negative predictive value. Acknowledging the limitations of this dataset and the challenges with testing our hypothesis, we conclude that focal splenic lesions should raise the suspicion of high grade transformation in follicular lymphoma and may identify a subset of patients that could benefit from anthracycline based chemotherapy.
Cunningham: Amgen: Research Funding; AstraZeneca: Research Funding; Bayer: Research Funding; Celgene: Research Funding; Merrimack: Research Funding; Mediummune: Research Funding; Merck Serono: Research Funding; Sanofi: Research Funding. Chau: Eli-Lilly: Other; Amgen: Research Funding; MSD: Other: Advisory board; Bristol Meyers Squibb: Other: Advisory board; Sanofi Oncology: Research Funding; Roche: Other: Advisory board; Sanofi Oncology: Other: Advisory board; Janssen-Cilag: Research Funding; Bayer: Other: Advisory board; Gilead Science: Research Funding; Pfizer: Honoraria; Eli-Lilly: Research Funding; Five Prime Therapeutics: Other: Advisory board; Merck-Serono: Research Funding; Novartis: Research Funding; Taiho: Honoraria. Iyengar: Gilead Inc: Honoraria; Janssen: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal